Something Old, Something New, Something Borrowed, and Something Blue Cross and Blue Shield of Texas
LATEST NEWS
COVID-19 Testing Of Non-Emergent Patients Seeking Non-Covid-19 Care, Elective Surgery Or Elective Procedures: Standard Of Care And Liability Risks
Two questions were posted on an American Health Law Association listserv as follows: “Not all hospitals and ASCs are testing patients before surgical procedures. What is the standard of care? Are these facilities potentially liable for risk to health care providers...
Physicians and Hospitals Criticized for Hoarding and Illegal Prescribing of Unproven Coronavirus Treatments
Physicians and hospitals criticized for hoarding and illegal prescribing of unproven coronavirus treatments; State pharmacy boards respond by issuing rules to curtail use of chloroquine and hydroxychloroquine as a preventative and to ensure availability for lupus and...
Bridal Shop’s Ebola Claim Fails Against Dallas Hospital
The Supreme Court of Texas has dismissed an Ohio bridal shop's negligence claim against a Dallas hospital for allowing a nurse who had been exposed to the Ebola virus to visit the shop leading to its closing.[1] The court ruled the claim was a "health care liability...
Are There Texas Rules On EE/IC Misclassification?
The employee/independent contractor misclassification question above was asked as part of a Q&A in a nationally published guide to Texas employment laws and rules. The answer was “Generally, no.” from a labor and employment law firm with several Texas offices....
Physician Employment Contracts Troublesome Terms Whether Starting or Continuing A Medical Career
For graduating residents and fellows, their first physician employment contract may be received with emotions of joy and trepidation. The contract is typically lengthy, contains multiple restrictions on the physician’s practice of medicine, and legally complex.
CONTACT LEW
THE OFFICE
The traditional rhyme for what a bride should wear at a wedding is adapted below for health care law purposes to recent litigation between out-of-network health care providers and health plans; audits of claims denials; litigation regarding use agreements for health care facilities and services; and a Blue Cross and Blue Shield of Texas contract mini-review.
Something Old. Litigation over routine waivers of deductibles and coinsurance between health plans and out-of-network (OON) health care providers is 25+ years old, dating from CIGNA’s spat with a chiropractic provider who routinely waived the patient’s OON financial responsibility in Kennedy v. Connecticut General Life Ins. Co., 924 F. 2d 698 (7th Cir. 1991). Marking this silver anniversary, CIGNA sued Virginia-based Health Diagnostic Laboratory, Inc. (HDL) on October 15, 2014 for $84 million over its “phantom rates” and “fee forgiving” scheme. HDL’s OON laboratories allegedly lured patients from CIGNA-administered or insured health plans by promising not to collect any OON deductible or coinsurance obligation. Further, HDL promised not to seek payment from patients for any other portion of the labs’ bills the plans did not cover.
CIGNA charged that HDL misleadingly billed the plans at “exorbitant and unjustified ‘phantom rates’ – rates that misrepresented what HDL actually intended to collect”. Evidence included HDL labs’ brochures stating that CIGNA’s members would have no out-of-pocket (OOP) costs and should not pay their patient financial responsibility indicated on explanations of benefits because HDL assumed all risk of non-coverage.
CIGNA’s reasons for the lawsuit against HDL are familiar ones in OON waiver cases:
- The Exclusions and Limitations (E&L) policies of CIGNA’s health plans state the plans do not cover services that members are not billed, are not obligated to pay or would not have been billed except that they were covered under the plans.
- CIGNA’s plans require their members to pay their OON coinsurance. Coinsurance is intended to sensitize members to the true and higher cost of OON services and to ensure that they have a financial incentive to seek in-network providers and suppliers.
- HDL’s charges did not represent the actual amount that HDL intended to require, accept or collect as payment in full for its services. Since HDL told the members in advance of receiving services that they would have not have to pay cost-sharing amounts or any other charges not covered, CIGNA alleged the members did not incur OOP costs at all.
- HDL failed to disclose to CIGNA material information regarding the manner, extent and nature by which it waived required OON deductibles and coinsurance.
- CIGNA paid false and misleading claims that contained charges for lab services that were higher than the actual amounts HDL required plan members to pay for those services.
- HDL engaged in a fee forgiving scheme designed to waive CIGNA members’ cost-sharing amounts to entice the members to its labs. The scheme also enticed CIGNA’s members to breach the terms of their health plans by misleading them about their health care benefits and requirements to pay OON deductibles and coinsurance.
Speaking of CIGNA and “fee forgiving”, the pending litigation, North Cypress Medical Center v. CIGNA, (No. 12-20695) in the U.S. Fifth Circuit Court of Appeals, involves an OON Texas hospital that offered prompt payment discounts on the deductibles and coinsurance owed by the patients, reducing their OON financial responsibility to in-network levels. To keep the hospital from enticing its members to go out-of-network, CIGNA implemented an anti-fee forgiving policy that would paid the hospital based on what it actually billed the OON patient rather than the charges billed to CIGNA. Thus, CIGNA deliberately underpaid OON services in which a patient’s portion of financial responsibility had been waived or reduced. CIGNA limited payments to $100 per claim regardless of the actual value of the hospital services.
Without the OON financial disincentives, CIGNA argued that its members would go to North Cypress and drive up the costs of providing benefits. CIGNA claimed that the prompt payment discount program did not require the patients to pay anything more than the discounted amount. Therefore, the patients incurred no OOP costs and no injury as a result of alleged CIGNA underpayments. Without an injury, the patients had no right to sue CIGNA and had no right to sue assignable to the hospital. CIGNA insisted that North Cypress must collect or sue for the patient’s OON cost sharing before demanding that CIGNA pay the hospital for covered services.
North Cypress sued CIGNA for several violations of ERISA including:
- Underpayment of members’ promised benefits,
- Breach of fiduciary duties,
- Failure to provide a fair and full review of benefit claims, and
- Failure to abide by the federal claims procedure regulation.
By counterclaims, CIGNA alleged North Cypress:
- Lacked standing under ERISA as an assignee because the patients had not suffered any loss or injury as a result of CIGNA’s underpayment to the hospital,
- Defended its reduced payments as consistent with E&L policies that entitled plans to pay based upon the amount the patients paid for the hospital services under the prompt payment discount, and
- Owed millions of dollars of overpayments that predated CIGNA’s anti-fee forgiving policy.
The federal court for the Southern District of Texas granted CIGNA summary judgment on the ERISA standing issue and its interpretation of its E&L policies, and dismissed the remainder of both parties’ claims to what overpayments or underpayments were owed.
In an amicus brief filed in October, 2013, and again in oral argument in April, 2014, the U.S. Department of Labor (DOL) stated the district court erred in dismissing North Cypress’s benefit claims for lack of ERISA standing. The DOL stated that the hospital has constitutional standing to sue for denied benefits under ERISA as an assignee of CIGNA’s members. Regardless of whether North Cypress is likely to collect from or sue CIGNA’s members directly for their OON financial responsibility, the DOL argued the members are injured because they have:
- an unextinguished debt for the hospital’s services; and
- a statutory right to have their promised and ERISA-protected benefits paid in accordance with terms of their plans and the DOL claims procedure regulation.
According to the DOL, CIGNA violated the “full and fair” review requirement of the claims procedure regulation by its refusal to pay any amount over $100 per claim regardless of its applicable plans’ provisions or the individual circumstances of the claims. The DOL stated that CIGNA’s insistence that North Cypress sue or threaten to sue members before submitting claims to CIGNA “defies common sense and undermines ERISA’s protective purposes”. The relevant injury to the members was CIGNA’s refusal to pay benefits at the time of assignment, and not whether an injury occurred after assignment because the hospital did not seek payment for OON deductibles and coinsurance.
As we wait the Fifth Circuit’s decision, a similar case attracting a DOL amicus brief and oral argument, Spinedex Physical Therapy v. United Healthcare, (12-17604) in the U.S. Ninth Circuit Court of Appeals, was decided on November 5, 2014. The appellate court upheld an OON provider’s ERISA right to sue United Healthcare (UHC) on behalf of patients for claims denied due to the provider’s failure to seek payment for OON deductibles and coinsurance.
Regardless of upfront waivers or a promise not to collect the patients’ financial responsibilities, the Ninth Circuit held a valid patient assignment of plan benefits that contained a patient’s legal obligation to pay for the services establishes the provider’s right to sue for payment from an ERISA-governed health plan. The Ninth Circuit noted that no federal appellate court had ever ruled that patients have not suffered an injury-in-fact due to a provider’s waiver or promise not to collect OON deductibles and coinsurance.
According to the opinion, the UHC plan members had the legal right to seek payment from the plan for the charges by the OON provider, and the provider assignee took from patient-assignors what rights they had at the time of assignment. But, the Ninth Circuit did not address whether UHC is entitled to deny claims, or assert overpayments, because of Spindex’s failure to bill or collect OON deductibles and coinsurance.
The three lawsuits are representative of claim denials for waivers or promises not to collect OON deductibles and coinsurance. Spindex supports the position that an OON provider with assignments of benefits cannot be denied plan payments if assignments state the provider’s right to bill the patients for the deductibles and coinsurance–regardless of whether the provider actually bills or collects.
However, providers should be aware that OON, waiver, assignment and billing/collection strategies and practices may be affected in different and conflicting ways by:
- ERISA and DOL regulations,
- State insurance codes and insurance fraud laws,
- State deceptive trade practices laws and advertising rules of state medical boards,
- State anti-assignment laws or anti-assignment provisions in plan contracts,
- Assignment of benefits provisions that do not effectively assign rights to sue for a plan’s breach of fiduciary duty under ERISA,
- Exclusions and limitations, exhaustion of administrative remedies and other provisions of health plan documents, and
- Other circumstances involving claims for benefits.
Prior to a decision to pursue an OON strategy involving waivers or no billing/collection of deductibles and coinsurance, health care providers should seek counsel from a health law attorney experienced in such matters.
Something New. The DOL’s Employee Benefit Security Administration (EBSA) conducts health plan audits for compliance under ERISA and the Affordable Care Act (ACA) to determine if self-insured and fully-insured health plans are making the ACA-mandated changes to plan design and communications to plan members. EBSA will now also investigate cases of improper denial of healthcare claims by plan administrators. EBSA believes a large number of claims are denied but few are appealed. Concern also exists that adequate communications about the revised claims appeal process has not been given to plan members.
EBSA audits of health plans may target benefits claims denied as:
- Unnecessary emergency room care,
- Experimental or investigational treatments,
- Unnecessary extensions of length of stay,
- Medically unnecessary,
- Excluded/non-covered services, or
- Charges that are not usual, customary and reasonable.
Health plans also have potential liability for breach of their fiduciary responsibilities for improperly denied claims.
Medicare also has something new for physicians—denial of their professional services claims without an audit if the hospital’s inpatient claim is denied for medically unnecessary admissions or procedures. Transmittal 541 (issued after CMS annulled earlier Transmittals 505, 534, 537 and 540 on the same subject), Medicare Program Integrity Manual, Section 3.2.3, allows the Medicare Administrative Contractors (MAC) and Zone Program Integrity Contractor (ZPIC) to have the discretion to deny other “related” claims submitted before or after the claim in question. If documentation associated with one claim can be used to validate another claim, those claims are considered “related”. The MAC and ZPIC are to await CMS approval prior to initiating requested “related” claims review.
Two CMS-approved examples of denial of a “related” claim occur when:
- The Part A inpatient surgical claim is denied as not reasonable and necessary, the MAC may recoup the surgeon’s Part B services.
- The patient’s history and physical (H&P), progress notes or other hospital record documentation does not support the medical necessity for performing the procedure, post-payment recoupment may occur for the performing physician’s Part B service.
Consequently, physician claims may be automatically denied if the hospital’s inpatient claim is denied—all based entirely on the documentation in the hospital’s record. Hospitals and physicians should ensure that all required documentation is in the hospital’s record to support medical necessity for the inpatient admission and procedure—including documentation from the physician’s office records.
MACs and ZPICs are not required to request additional documentation for the “related” claims before denying them. “Related” claims may be denied automatically or after manual review. Hospital and physician appeals of denied “related” claims are processed separately. Remember that Recovery Audit Contractors (RACs) may request approval to review “related” claims through their standard issue approval process. RAC reviews are primarily automated but may include complex reviews of hospital surgical claims.
As with the two midnights rule for inpatient status, the MACs will have the ability to change the physician’s evaluation/management code from inpatient to outpatient if inpatient status is not medically necessary. Thus, the hospital’s claim is subject to denial but the physician’s claim can still be recoded and paid. If there was a deficit in documentation in the hospital record, the hospital can submit a claim before the expiration of timely filing and also receive Part B payment as if the case had been outpatient. Medicare patients are liable for their usual Part B financial liability. The difference between Part A and Part B patient cost-sharing amounts may entail a refund to or greater cost-sharing for the patient.
However, if the medical necessity of the surgical procedure is the reason for denial, the physician’s Part B claim is denied completely as is any hospital claim.
To avoid inpatient and related claim denials, hospital and physicians should consider revisions to medical necessity and documentation policies and procedures for inpatient admissions and surgical procedures that address physician office documentation and records.
Something Borrowed. Higher fees paid to hospitals, ambulatory surgery centers (ASCs) and other licensed health care facilities have motivated some physicians to develop schemes to capture part of the facility payments to augment their lower professional services fees. Due to over-building of operating room capacity, one favored scheme in Texas has been the use agreement. ASCs with unscheduled operating rooms entered into contracts with surgical groups granting them the right to use the ASC premises, equipment, personnel and services. The use agreement declared that the right to use did not constitute an interest, estate or lease of the ASC’s real property or any change or transfer of the ASC’s license.
The surgical group typically paid the ASC a use fee equal to 45% of the net monthly collections plus a fixed per case fee. No Medicare, Medicaid, Blue Cross and Blue Shield (BCBS) and workers compensation (WC) patients were accepted as patients—use agreements only pertained to patients from self-insured health plans or with commercial health insurance. Government, BCBS and WC payers were excluded because laws, regulations and contracts limited facility payment to ASCs participating in those programs or plans.
Eventually, commercial payers realized that they were paying facility fees to a surgeon or surgical practice that had no ASC license. Payers sought refunds and/or sued for their past payments based on violations of Texas ASC laws and regulations that prohibited:
- More than one provider from using the same ASC facility,
- Transfer/assignment of ASC licenses, or
- Ceding ASC control over surgeries to the surgeons or surgical groups.
ASCs countered that there were no laws, regulations or cases addressing use of ASC premises, equipment, personnel and services. ASCs also believed that splitting a facility fee with the surgical group was not a payment for patient referrals in violation of the Texas Patient Non-Solicitation Act, Tex. Occ. Code, Sec. 102, as the surgical groups were paying fair market value use fees to the ASCs. Use agreement cases have either been settled or remain pending in court.
A recent twist on the use agreement—minus the use of the facility and billing in physicians’ names– involved three medical clinics that borrowed the license and Medicare provider number of 4-bed Cleveland Imaging and Surgical Hospital, Cleveland, Texas. The hospital did not own or operate the clinics, and the clinics were not granted provider-based status. Three physicians who owned the hospital owned one clinic. The clinics used the hospital’s provider number and its emergency room and outpatient point of service codes to bill for services actually provided at the clinics. The hospital paid the clinics 85% of insurers’ payments to the hospital.
Alerted by Medicare’s threat to revoke the provider status of the hospital due to the high ratio of outpatients not being admitted for treatment, Aetna sued. The hospital had billed Aetna for over $9.2 million in ER and outpatient services actually furnished by the three clinics.
The Southern District federal court issued a decision in Aetna’s favor. The court ruled a use agreement cannot change the objective reality that the clinics were physician-owned clinics, not qualified to be hospitals, ERs or hospital outpatient clinics. According to the ruling, the physicians and clinics may not contract to use a hospital’s billing codes to recover fees designed to compensate a hospital for expenses that it did not have. The court awarded Aetna $8.4 million for fictitious claims to be paid by the Cleveland hospital and the clinics. The court has not yet ruled on fraud, negligent misrepresentation, unjust enrichment and civil conspiracy claims.
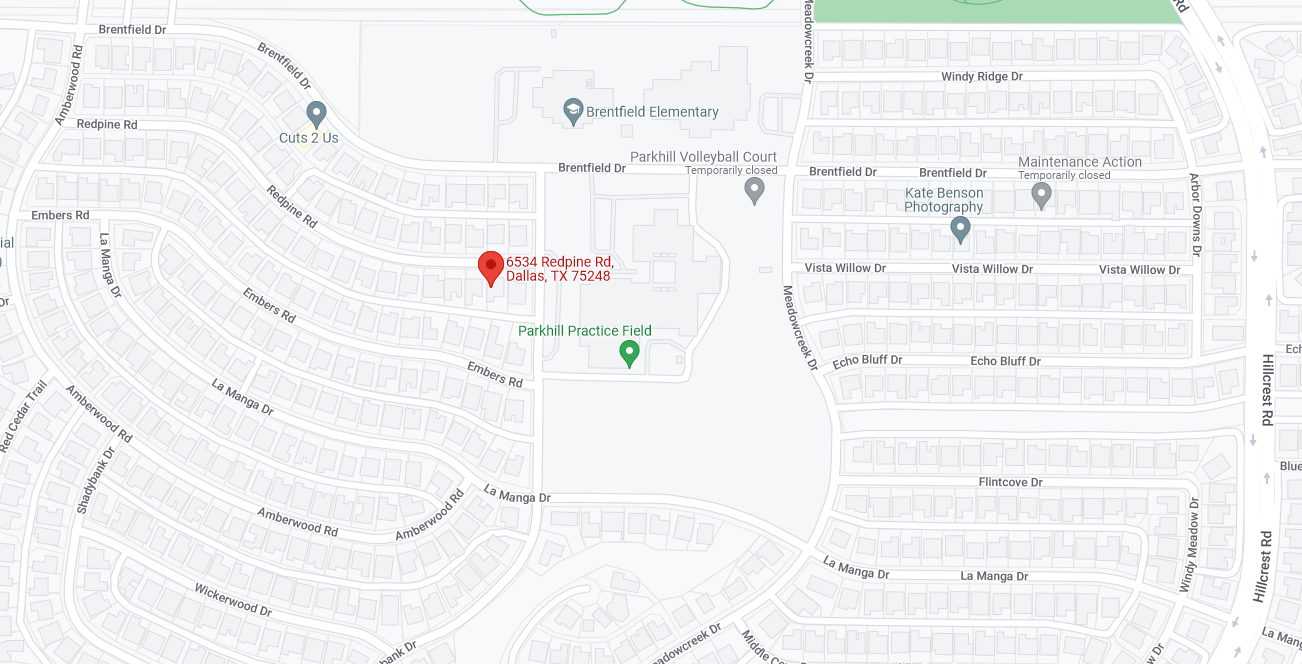
The use agreement scheme continues in other contexts by physicians and even non-providers who are able to schedule patients, see Image Connection, LLC v. United Healthcare Services, Inc. and Robin Brady, Case No. 3:2013cv04658, Northern District of Texas (Dallas), Nov. 22, 2013. Hospitals, ASCs and other health care facilities should consult their health law attorney when presented with a use agreement.
Something Blue Cross and Blue Shield of Texas. Managed care contracts are far from perfect with respect to drafting. These contracts may be defective or deficient due to incomplete, vague or inadequate details or descriptions, misplaced information or terms, errors, omissions, conflicts, inconsistencies, ambiguities or misleading provisions. No one expects managed care contracts to be models of clarity—but an unreasonable number of problems may disrupt the managed care organization (MCO)-provider relationship, increase legal work to correct the defects and increase costs. Much of managed care litigation involves interpretation of the meaning and scope of contract provisions. Key parts of the Blue Cross and Blue Shield of Texas (BCBSTX) contract for Medical Groups may cause such difficulties.
Vincent Martorana, a contract drafting expert, describes definitions as an efficient way to package a concept and to employ that concept repeatedly in a contract. Definitions explain to the parties what certain terms mean—and that should be all definitions contain. A common error in drafting definitions is placing obligations of the parties in a definition rather than in the proper contract provision. BCBSTX misplaces numerous obligations in the Definitions section that a health care provider may overlook.
In the definition of Medical Group, the contract states that, where applicable by context, Medical Group also means Medical Group Providers. BCBSTX then adds Medical Group shall require that Medical Group Providers comply with the provisions of this Agreement that are applicable by context to Medical Group Providers. There are 17 pages of provisions in the Medical Group Agreement that may, by context, apply to Medical Group’s physicians and licensed practitioners to perform but that BCBSTX does not identify.
Context may be the most inadequate word in the BCBSTX contract. By definition, context refers to sentences or provisions that immediately precede and follow the particular sentence or provision being interpreted. How much of the contract is context for any particular sentence or provision? Many managed care companies do away with this burdensome, time-consuming analysis of the context of every contract provision by use of a flow-down provision, joinder or addendum binding the individual physicians to the Medical Group’s obligations without making the physicians parties to the contract.
Other Medical Group obligations in the Definitions include:
- The required means of sending a “Notice” and when a Notice is “deemed received”;
- In-Network Services that do not require “Proper Referrals” pursuant to the Utilization Management Program;
- The content of a Proper Referral and Preauthorization; and
- Designation of BCBSTX or a licensed utilization review firm by a Health Plan to act as its utilization management agent (UM Agent), and that BCBSTX may further delegate its obligations to act as UM Agent to any other entity licensed or permitted to perform UM in Texas (omitting whether BCBSTX remains fully responsible for obligations, services and functions performed by such delegated UM Agent).
Inconsistencies between the managed care contract, the addenda, attachments and schedules and the provider manual may create major problems. A mechanism to address the discrepancy/conflict issue is to use a precedence provision that designates which documents supersede other documents. In the case of conflicting provisions, the attachments and addenda prevail over the BCBSTX Agreement, but the Agreement prevails over the Provider Manual.
The BCBSTX Agreement refers to itself, the Provider Manual, attachments to the Agreement, amendments to the Agreement, the Provider Manual and attachments to the Agreement, correspondence between BCBSTX and the Medical Group, Health Plans and Membership Agreements as sources of requirements for the Medical Group. Consistent with the computer age, BCBSTX also refers to its website as another source of requirements. Clinical policies and the verification of benefits process for guarantees that a particular service will be paid by BCBSTX (applicable to Health Plans subject to the Texas prompt pay legislation) are only found on the website and not in the Provider Manual.
The Dispute Resolution provision includes a mandatory arbitration for certain disputes. The provision requires the Medical Group waive participation in any class action against BCBSTX. No arbitration decision may require any adjustment in compensation or payments to the Medical Group respecting any dispute involving services rendered more than 18 months prior to the receipt of the initial notice, rather than the 4-year statute of limitations period. If the Medical Group disputes the appropriateness of claims adjudication, it has the burden of proof that the claims were adjudicated incorrectly. Even if the Medical Group offers proof or reasonable probability of incorrect adjudication, it has to pay for the administrative costs of BCBSTX into research of each claim that was not proven as incorrectly adjudicated adversely to the Medical Group. A Medical Group should give serious consideration to scrapping the Dispute Resolution provision from the contract in favor of litigation with a waiver of a jury trial.
Health care providers should know or suspect that there are problems in managed care contracts and their accompanying materials. Providers that fail to seek negotiation, clarification and/or correction of these contracts and materials do so at their own risk. No managed care contract provision provides additional compensation to a provider for additional work, burden and/or cost caused by problems of ambiguity, conflict, inconsistency, omission or error. Review of managed care contracts by an experienced health law attorney is important to identifying and resolving such issues.
© Copyright 2024
Designed by StarFlame Solutions, LLC